Every so often I am asked to give a talk on managing up and how to work with your Chairman, Division Head, or some other supervisor. In this mythical tale, I relate the story of Sid Arthur MD, a mere worker in the vineyard who aspired to great things, but most of all, inner peace and not to be scorched by Dragons. Perhaps you will find some interesting thoughts to consider. Namaste.
New Beginnings at the Crozer Keystone Health System: Crozer Emergency Medicine
I am very excited to announce that I will continue in my role as Emergency Medicine Chair for Drexel University College of Medicine. My new beginning will be as EM Chair for the Crozer Keystone Health System and the Regional Associate Dean for the Crozer Keystone Campus. Crozer is a regional campus for Drexel Med and has a 4 hospital system and an Emergency Medicine Residency and an Ultrasound Fellowship. Amazingly, I am also reunited with some of my displaced residents and former colleagues, and I will be bringing onboard some of the faculty from our residency at Hahnemann. To get me started, Dr. Mark Saks and I sat down and talked about the Health System and the EM Residency. Mark is the Program Director for Crozer EM, and a friend and former faculty at Hahnemann. He was the APD for our program at Drexel and founded the Crozer EM Residency 5 years ago. Mark is a Professor of Emergency Medicine at Drexel University College of Medicine. We talked about the established EM residency and ultrasound fellowship at Crozer and the great training that the residents and fellows are getting at the program. In my first month, I have already been so deeply impressed with the people in the department! Suffice it to say that I am thrilled and thankful to be part of this great crew and I am very excited to get started!
Now on to the Podcast!
The Hahnemann University Hospital Closure and What Matters: A Department Chair’s Perspective
My invited commentary on what happened to us at Hahnemann.
The Hahnemann University Hospital Closure and What Matters: A Department Chair’s Perspective
Even today, and I suspect for years, the closure of Hahnemann University Hospital will continue to have heartbreaking consequences. Physicians, nurses, and staff are all still enduring the after effects of the dissolution of our mission and purpose at Broad & Vine – to make our patient’s lives better. Lifelong relationships with our patients and our co-workers were shattered. Teachers and learners split apart. Ongoing personal financial losses continue for everyone that worked there – especially for the physicians and other providers who were not provided malpractice tail coverage and now may need to purchase a policy out of their own pocket. This photo is from the last day that we were all together. Hahnemann Emergency Medicine was a special place, like no other, and I miss it badly.

Click on the link below for the article in Academic Medicine and my thoughts on the matter and a timeline of events.
The Hahnemann University Hospital Closure and What Matters: A Department Chair’s Perspective
Abstract: The closure of Hahnemann University Hospital (HUH), which was announced on June 26, 2019, resulted in the most significant graduate medical education displacement in history, sending 570 residents to new institutions within a month of the announcement. Over 2,000 physicians, nurses, and staff lost their jobs. While seemingly predictable in retrospect, the closure came as a cataclysmic event to all involved. In this Invited Commentary, a Department Chair reflects on the lessons learned from these unprecedented circumstances. These lessons cover areas that are not a typical concern for faculty who are focused on teaching their trainees, but are worthy of their attention. Corporate and organizational structure, leadership, and financing of the hospital were critical determining characteristics of the failure. The role that the Accreditation Council for Graduate Medical Education and the Centers for Medicare and Medicaid Services played in this event were key stabilizers. However, their role in future events offer opportunities to play a more active role and alter how the next massive displacement unfolds, possibly preserving teaching programs. Highly competitive health systems should rethink non-collaborative strategies before allowing struggling institutions to succumb to market forces. Finally, a commitment by a hospital to the mission of academic medicine is a sacred trust with the faculty, trainees, and patients that it serves. It should not be undertaken by any enterprise that is not well resourced and equipped with the knowledge and expertise to meet this most serious of commitments.

Syncope, BVM in RSI, and post ROSC Cath Lab activation! Find out more by listening to our Drexel EM Journal Club for April 2019
Welcome to April Journal Club! Today we tackle the question of observing patients in the ED on a monitor after a syncopal episode, BVM ventilation and intubation, and whether to activate the cath lab immediately after ROSC. These issues represent dilemmas we face everyday in the ED and these articles help shed light on practice.
Duration of Electrocardiographic Monitoring of Emergency Department Patients With Syncope
Bag-Mask Ventilation during Tracheal Intubation of Critically Ill Adults
we also talk mention this article from 1970
Rapid induction-intubation for prevention of gastric-content aspiration. Which you can find free here
and finally
Coronary Angiography after Cardiac Arrest without ST-Segment Elevation
Hope you enjoy the podcast – and DON’T THROW OUT THE PEEP VALVE WHEN YOU OPEN A BVM KIT – USE IT!!!!
Ultra sensitive troponin, the HOUR rule, and Double Sequential Defibrillation: The Drexel EM Journal Club for March
First, a heartfelt shout-out to Drexel EM3 Dr. Alin Gragossian and her wonderful new blog. We cherish this wonderful friend and colleague and we miss her each and every day. Can’t wait for her to be back by our side (as she soon will be) dealing with our challenging EM cases! Her journey from the brink and back again is unique and inspiring – and she is an excellent writer. Get back here soon, Alin!!!
Subscribe to updates and check it out here: a change of heart

Our March Journal Club looks at three articles of interest:
Ultrarapid Rule-out for Acute Myocardial Infarction Using the Generation 5 Cardiac Troponin T Assay: Results From the REACTION-US Study.
Hospital Observation Upon Reversal (HOUR) With Naloxone: A Prospective Clinical Prediction Rule Validation Study.
Double sequential external defibrillation for refractory ventricular fibrillation out-of-hospital cardiac arrest: A systematic review and meta-analysis.
Reading these three articles will help you with the clinical challenges we are tackling this month: Will the new ultra sensitive troponin change your practice? When can an opioid overdose reversed with naloxone can go home? How do you treat refractory ventricular fibrillation – can double sequential defibrillation make a difference? Listen in here to find out what we think – and see you at Journal Club!
Decision Science Rounds: Can we predict early deterioration in hospitalized patients?
In this podcast, I am joined by Ryan Arnold M.D. and Muga Capan Ph.D. who are directing our newly formed Center for Healthcare Analytics and Decision Science. They put together a graduate student team of Andrew Armstrong, Devanshi Dholakia, Karen Nwal, Karan Gandhi, Mallika Mhapankar, Matthew Shaw, Mihir Chheda, Parth Girme, Sharath Chandra, Zoya Khalife to analyze the hospital rapid response database created by EM Resident Mark Ramzy MD. Their goal was to use decision science tools to try to determine if there was a pattern that predicted early v late rapid response in patients admitted through the ED. The hope was that characteristics, identifiable in the ED, could predict who would deteriorate early. There was a pattern – but not what you’d expect! Listen in to find out more!

Drexel Business Dragons working with Drexel Medical Dragons!
November Journal Club for Drexel EM: Appy’s, Oxygen, and CT for Seizures

Reading the literature is not just a part of residency training – it’s an important habit of EM physicians who have an evidence based practice!
Here’s the articles we are reviewing!
Is every appendicitis case a surgical emergency – maybe not!
Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis
Oxygen – too little is not so good. What about too much? Well that’s another matter…
Emergency department neuroimaging for epileptic seizures This article looks at whether imaging is really required in patients who have a seizure with a known history of epilepsy and no other concerns really need a head CT
Enjoy – thanks for listening as always and see you at the boathouse!
Find the podcast here:
Podcast for November Journal Club Drexel EM
Epinephrine, agitation, and pediatric DKA – important articles for August Journal Club
Clinical Trial of Fluid Infusion Rates for Pediatric Diabetic Ketoacidosis
Years in the making, this study finally establishes that a rapid resuscitation approach to pediatric DKA is appropriate and is not responsible for cerebral edema.
Intramuscular Midazolam, Olanzapine, Ziprasidone, or Haloperidol for Treating Acute Agitation in the Emergency Department
Single agents for acute agitation – is one better than the other?
A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest
Epinephrine saves lives, but at what cost?
Enjoy the podcast below:
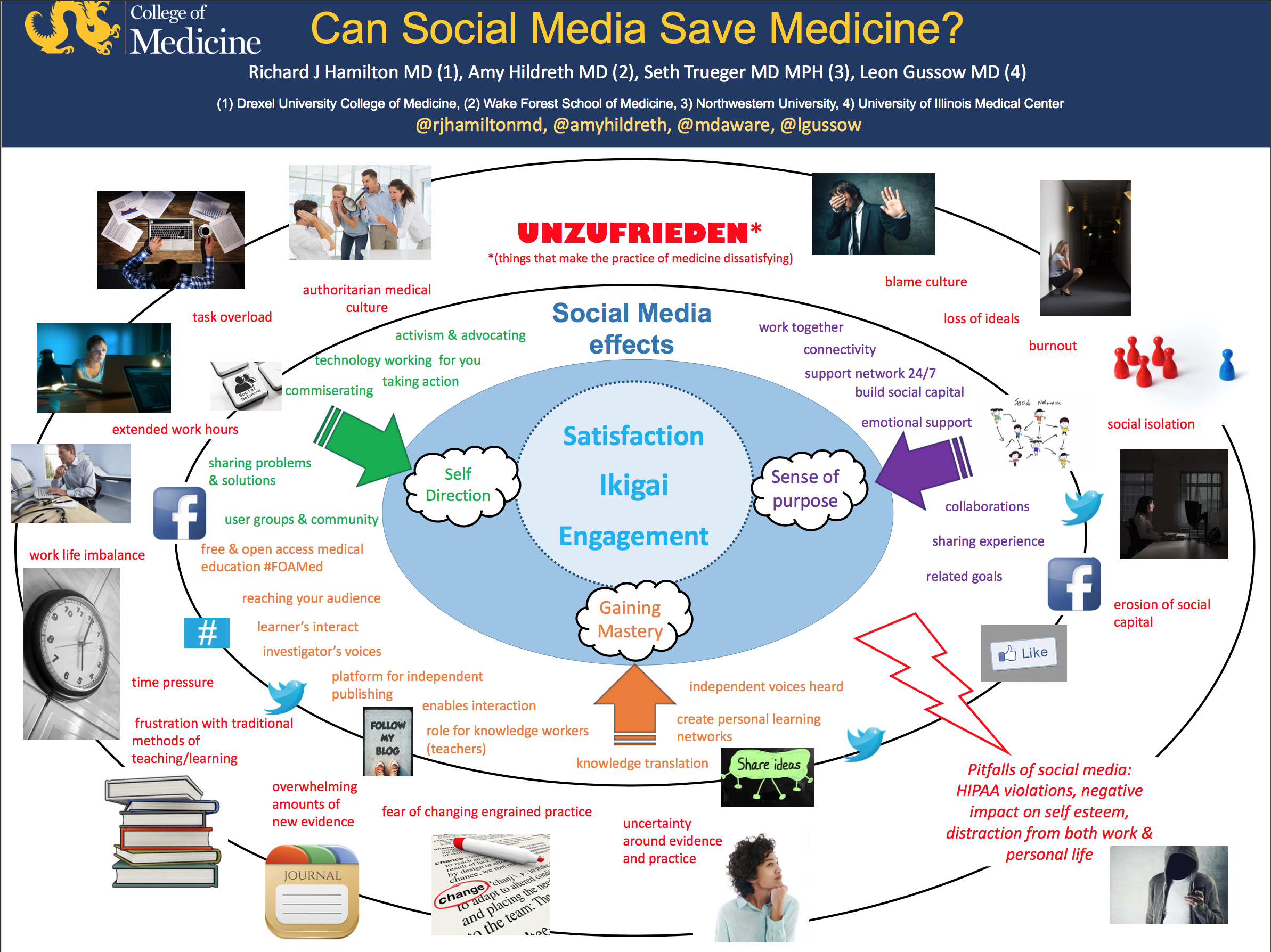
The Blue Zones in Medicine: Where are they? The role of social media – can social media save medicine? Special thanks to @amyhildreth @MDaware @lgussow
soundcloud.com/rjhamiltonmd/blue-zones-in-medicine
Blue Zone in Medicine Role of Social Media Richard Hamilton presented at the AAMC CFAS meeting with the support of AACEM – thank you!